Odontogenic Rhinosinusitis
 Odontogenic rhinosinusitis is defined as sinusitis induced by a dental lesion. The common etiologies include periapical and periodontal disease, odontogenic lesions and iatrogenic and traumatic causes. Iatrogenic causes include complications of tooth extractions, implants, sinus floor augmentation, osteotomies and other orthodontic surgery, and a foreign body reaction to either the root canal sealant or filling material used in root canal therapy. A significant amount of literature is dedicated to complications associated with dental implants and sinus lifts. The reported incidence of rhinosinusitis resulting from sinus augmentation is 0-27% (1). However, when strict criteria are used to define rhinosinusitis, the incidence is 4.5%. Approximately 1/3 of these patients will progress from acute to chronic rhinosinusitis. Chronic rhinosinusitis requiring surgical intervention from sinus augmentation is reported to occur in 1.3% of patients (1). Sinus inflammation or swelling on pre-augmentation CT imaging is a statistically significant risk factor for post procedure acute or chronic rhinosinusitis (2).These are patients who would benefit from a ENT evaluation prior to their “sinus lift” procedure.
Odontogenic rhinosinusitis is defined as sinusitis induced by a dental lesion. The common etiologies include periapical and periodontal disease, odontogenic lesions and iatrogenic and traumatic causes. Iatrogenic causes include complications of tooth extractions, implants, sinus floor augmentation, osteotomies and other orthodontic surgery, and a foreign body reaction to either the root canal sealant or filling material used in root canal therapy. A significant amount of literature is dedicated to complications associated with dental implants and sinus lifts. The reported incidence of rhinosinusitis resulting from sinus augmentation is 0-27% (1). However, when strict criteria are used to define rhinosinusitis, the incidence is 4.5%. Approximately 1/3 of these patients will progress from acute to chronic rhinosinusitis. Chronic rhinosinusitis requiring surgical intervention from sinus augmentation is reported to occur in 1.3% of patients (1). Sinus inflammation or swelling on pre-augmentation CT imaging is a statistically significant risk factor for post procedure acute or chronic rhinosinusitis (2).These are patients who would benefit from a ENT evaluation prior to their “sinus lift” procedure.
Treatment of routine sinusitis consists of saline irrigations, topical and systemic decongestants, antibiotics, topical and systemic steroids and allergy treatment. Antibiotics are used to treat acute rhinosinusitis and acute exacerbations of chronic rhinosinusitis. The specific antibiotic used is based on common microbiology patterns or the result of endoscopically-guided cultures. Recommended first-line antibiotics include Augmentin, high-dose amoxicillin, and extended spectrum cephalosporins. Surgery for acute or chronic rhinosinusitis is usually a last resort after maximal medical therapy has failed.
Patients with odontogenic rhinosinusitis present a unique challenge to the otolaryngologist. The diagnosis is frequently delayed. A dental source for the sinus infection is frequently not considered until after both medical and surgical therapy has failed to resolve the patient's symptoms. A primary cause for the delay in diagnosis is the failure of the radiologist and ENT physician to adequately assess dental pathology on CT imaging. In a 2010 retrospective case series involving 21 patients with known odontogenic rhinosinusitis, the initial radiology report failed to mention radiographic findings of dental pathology in 14 (or 67% percent) of the patients (3). Therefore, the otolaryngologist should have experience diagnosing dental pathology on CT imaging studies. In addition, there are symptoms which suggest an odontogenic source for the infection in the patient presenting with rhinosinusitis. First, the large majority of patients will present with unilateral symptoms. This means that the patient will complain of nasal discharge, cheek pain, dental pain or nasal obstruction primarily on one side. Another unique symptom to odontogenic rhinosinusitis is a foul smell noted by the patient. In a review of 76 patients with known odontogenic rhinosinusitis, 33 or 43% reported a foul smell (3,4,5).
In addition to early diagnosis, a successful outcome of odontogenic rhinosinusitis requires appropriate antibiotic therapy based on the common microbiology findings of a mixed polymicrobial infection. Like other odontogenic-induced infections, first-line antibiotic coverage for ORS is clindamycin. Additionally, successful treatment depends on eliminating the source of the infection. This requires early involvement of the dental health professional. In general, dental procedures take precedence over the ENT procedures. Situations where ENT surgery would precede dental surgery include the following:
- A complication of rhinosinusitis requiring emergent surgery.
- Sinus surgery in an infected maxillary sinus performed prior to closure of an oral antral fistula to increase the chance of success.
- Sinus surgery for pre-existing sinus disease prior to sinus augmentation (6).
The most important aspect of successful treatment consists of good coordination of care and communication between the dentist and ENT physician. The ENT physician should make contact with the dentist, endodontist, or oral surgeon prior to proceeding with surgical therapy.
- ENT assessment in the integrated management of candidate for (maxillary) sinus lift. Pignataro L, Mantovani M, Torretta S, et al. ActaOto rhino laryngolItal 28:110–119, 2008.
- Late signs and symptoms of maxillary sinusitis after sinus augmentation. Manor Y, Mardinger O, Bietlitum I, et al.OralSurg Oral Med Oral Pathol Oral RadiolEndod 110:e1–e4, 2010.
- Clinical aspects of odontogenic maxillary sinusitis: a case series. Longhini AB. Ferguson BJ. International Forum of Allergy & Rhinology. 1(5):409-15, 2011 Sep-Oct.
- Microbiology of acute and chronic maxillary sinusitis associated with an odontogenic origin. Brook I. Laryngoscope. 115(5):823--‐5, 2005 May.
- Late signs and symptoms of maxillary Sinusitis after Sinus augmentation. Manor Y, Mardinger O, Bietlitum I, et al. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 110:e1-e4, 2010.
- The characteristics and new treatment paradigm of dental implant-related chronic rhinosinusitis. Chen YW, Huang CC, Chang PH, Chen CW, Wu CC, Fu CH, Lee TJ. Am J Rhinol Allergy. 2013 May;27(3):237-44.
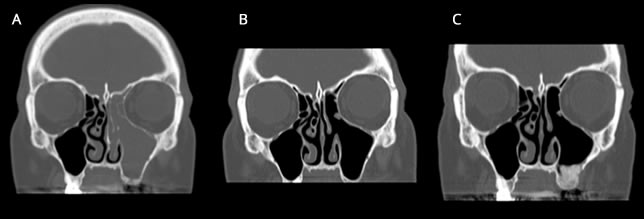
A 51 year old female presents with one year of left facial & tooth pain, left nasal obstruction, postnasal drainage and headaches. Past dental history is significant for RCT of teeth 10 & 11, apicoectomy of tooth #10, and tooth implants #12 & 13. The implants failed and she developed an oral antral fistula after removal of the implants and debridement of necrotic bone. Coronal CT image demonstrating severe left maxillary and ethmoid sinus disease (A). A coronal CT (B) 2 months after ethmoid and maxillary sinus surgery showing complete resolution of sinus disease. Several months later, she underwent a successful sinus lift with implantation. A coronal CT image demonstrating ossification of maxilla after sinus augmentation (C).
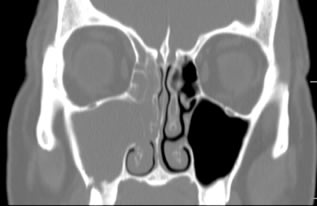
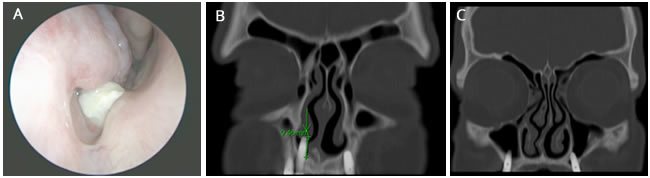
A 70 year old male with postnasal drainage presents with a right nasal cavity mass demonstrated on nasal endoscopy (A). A yellow discharge is associated with the object. A coronal CT image demonstrates extrusion of a dental implant 9.5mm into the right nasal cavity consistent with the foreign body (B). Additional implants are extruding into the maxillary sinuses without radiographic disease (c).
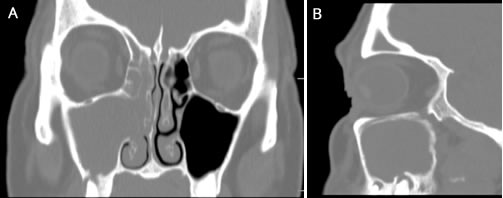
A 69 year old female presents with 12 months of brown-yellow nasal drainage, mild right facial pressure, right nasal congestion and a foul taste and smell. She presented to her general dentist 3 months prior to her ENT consultation with a right gingival buccal lesion that resolved with clindamycin. A coronal CT image of the paranasal sinuses demonstrates maxillary and ethmoid sinusitis ipsilateral to right maxillary periapical disease (A) with buccal plate and maxillary sinus floor boney erosion. A sagittal image through the right maxillary sinus shows periapical disease of teeth #2 and 3 (B).