Rhinosinusitis 101 - What are the Sinuses?
Rhinosinusitis Resources
- What are the Sinuses?
- What is Sinusitis?
- What are the signs and symptoms of Rhinosinusitis?
- What are Nasal Polyps?
- Why do I have Sinusitis?
- Why Do I Have Chronic Sinusitis?
- Why Do I have Acute Sinusitis?
- Thyroid Eye Disease and the Sinuses
- Our Philosophy
What are the Sinuses?
Anatomy and Physiology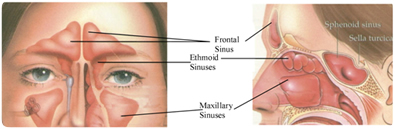
The sinuses are air filled cavities in the skull. There are 4 sets of sinuses. The frontal sinuses lie above the eye and in front of the brain on each side. The ethmoid sinuses are a group of smaller air cells clustered between your eyes. The maxillary sinuses lie underneath each eye and the sphenoid sinuses lie in the center of your head, underneath the brain. All of the sinuses have openings which communicate with the inside of the nose. The maxillary sinuses are the first to form during human development in the womb. They are very small at birth and continue to grow throughout childhood. The ethmoid sinuses are also present at birth but small. The sphenoid and frontal sinuses are not visible on x-rays at birth but continue to grow into childhood. About 10% of the population are lacking a frontal sinus on one side and around 4% of the population do not have frontal sinuses.
Certain structures inside the nose are closely related to the sinuses. The internal side wall of the nasal cavity on each side has 3 sausage shaped protuberances. These are called turbinates (inferior, middle and superior turbinates). The turbinates are bony outgrowths which are lined by a thick mucous membrane. They act as “radiators” or the “HVAC” (heating/ventilation/air-conditioning) system for the nose with the purpose of warming, humidifying and filtering air for the lungs. The turbinates have a very rich supply of blood vessels underneath the mucous membrane and this allows for heat to be transmitted to the nasally inhaled hair. They are also coated with a thin, wet mucous coating which gives off water vapor and humidity to the nasally inhaled air. The mucous coating also traps foreign particles in the air (dust, pollen, mold spores, smoke particles, air pollution, carpet fibers, insects, etc) and thus filters the air before it gets to the lungs. The turbinates are necessary for normal nasal function but they can malfunction or become problematic in certain conditions (colds, allergy flares, sinus infections, chemical irritation, congenital enlargement). During these conditions, the turbinates are swollen and cause congestion and obstructed nasal breathing or perhaps even blockage of the sinus drainage pathways. Medications designed to control the swelling may be effective in reversing the process. Sometimes the turbinates are irreversibly swollen and procedures are required to reduce their size.
The sinuses are lined with a moist mucous membrane similar in appearance to that on the inside of your mouth. This moist, pink mucous membrane is called respiratory mucosa. It is constantly secreting mucous. The mucous is continuously “swept” out of the sinuses by microscopic hairs lining the mucosa. These tiny hairs also line the nasal passages and are called cilia. In a normal, healthy nose clear mucous is produced in the nose and sinuses and is swept out of the sinuses through small drainage holes into the nasal passages. In the nose, the mucous gets transmitted by the cilia to the nasopharynx (the back of the nose, just above the throat). Here it is transmitted to the throat and swallowed. This is the normal process and as long as the mucous is not over produced or abnormally thick, we don’t notice the process of mucous clearance and swallowing. During allergy flare ups, colds, sinus infections , exposure to smoke or air pollution or in particularly dry environments (airplane, desert climate) the mucous becomes thick or overproduced. This interferes with the clearance from the sinuses and nose. In addition to the mucous being thick and difficult to clear, the cilia do not function normally during the above mentioned conditions. Therefore, the mucous can accumulate in the nose and sinuses, causing congestion and pressure and ultimately the mucous can become secondarily infected by bacteria.
The function of the paranasal sinuses remains largely unknown. Many theories exist on the reason we have sinuses. They include:
- Functioning as resonance chambers for speech
- Supplying conditioned air to diffuse with inhaled air in the nose
- To assist with the sense of smell
- To protect the brain (by acting as a “crumple zone” during blunt trauma to the face and
forehead) - To lighten the skull (hollow spaces in the skull instead of solid bone)
What is Sinusitis?
Sinusitis means inflammation of the mucous membrane within the sinuses. Figuring out the cause of sinusitis can be challenging. Sometimes it can be straightforward, such as in the setting of acute sinusitis (usually viral or bacterial). Uncovering the etiology of chronic sinusitis can be more difficult. Several theories exist and the cause is probably multifactorial (overactive immune response to inhaled foreign particles, air quality in the patient’s environment, bacteria in the nose and sinuses, fungal spores in the sinuses and variations in sinus and nasal anatomy). See “Why do I have Sinusitis?” below.
What are the signs and symptoms of Rhinosinusitis?
There are many symptoms suggestive of Rhinosinusitis. To help with making a diagnosis of sinusitis, the symptoms are divided into “major symptoms” and “minor symptoms”.
"Major" Symptoms
- Nasal obstruction
- Facial congestion or fullness
- Facial pain or pressure
- Thick & discolored drainage
- Change in taste or smell
"Minor" Symptoms
- Fever
- Fatigue
- Bad breath
- Headache
- Tooth pain
- Cough
- Ear pressure
One of the following combinations is required for a diagnosis of sinusitis
- At least two of the major symptoms or
- One major symptom and two minor symptoms
The diagnosis of sinusitis should be confirmed with nasal endoscopy and/or a CT scan. On the nasal endoscopy purulent (infected) discharge and swelling of the sinus drainage pathways indicates sinusitis. The diagnosis is also confirmed if the CT scan reveals sinuses filled with thick mucous or sinuses that are lined by thickened mucous membranes.
Sinusitis is further characterized by the duration of the condition. Acute sinusitis is present for four weeks or less. Signs and symptoms present between 4 and 12 weeks qualify as sub-acute sinusitis. Sinusitis present for greater than 12 weeks is considered chronic sinusitis.
Acute Sinusitis: < 4 weeks
Sub-acute Sinusitis: 4-12 weeks
Chronic Sinusitis: > 12 weeks
Acute Sinusitis is usually characterized by intense symptoms for several days. This variation of sinus inflammation usually results from viral or bacterial infection. Sometimes a viral infection precedes an acute bacterial sinusitis. Viral sinusitis usually accompanies a cold and the patient may have “flu-like” symptoms. Upper respiratory viral infections usually resolve in less than one week with supportive measures such as rest, hydration, acetaminophen, nasal or oral decongestants and nasal saline rinses. Bacterial acute sinusitis usually manifests with fever, facial pain, white or green discharge from the nose and nasal obstruction. Antibiotics and supportive care are helpful in reducing the severity and duration of acute sinusitis.
What are Nasal Polyps?
Nasal polyps are gelatinous, non-cancerous masses which grow along the sinus outflow tracts. They resemble peeled grapes. They usually form in response to persistent nasal and sinus inflammation. The exact cause of nasal polyps is not known although some researchers suspect they form in the setting of an overactive immune response to inhaled particles. Nasal polyps usually grow in clusters, like grapes. Occasionally a single large polyp will grow out of one sinus and extend into the nose. Although polyps are more common than nasal and sinus cancers, any growth in the nose should be evaluated by an ear, nose and throat physician to rule out the possibility of a cancer.
Why do I have Sinusitis?
Doctors may not always have the answer to this question but we do know that certain conditions put you at risk for sinus inflammation.
Predisposing factors
- Viral Illness
- Environmental irritants/poor air quality (cigarette smoke, ozone, sulfur dioxide, carbon monoxide, lead and other particulates in the air)
- Allergy
- Anatomy (Structural blockage of sinus outflow)
Why Do I Have Acute Sinusitis?
In otherwise healthy individuals with acute sinusitis the inflammation is usually due to a viral or bacterial infection. The bacterial infection usually results from obstructed sinus drainage pathways (swelling of the mucous membrane at the drainage opening can obstruct the sinus opening causing mucous buildup in the sinus). The cause of swelling at the sinus opening could be viral inflammation, an allergy flare, obstructing anatomy in combination with either viral or allergic inflammation, tumor or polyp growth, or any disorder causing mucous membrane swelling.
Stagnant mucous within the sinus can easily become infected with bacteria. The bacteria that are residing in the nose and sinuses can flourish in the thick mucous which acts as a culture medium. The body sends bacteria fighting immune cells to the sinus and substances are released into the area of the sinus mucous membrane which cause swelling and more mucous production. This can become a vicious cycle of mucous build-up, infection of that mucous, mucous membrane inflammation and swelling, sinus outflow obstruction and more mucous build-up, etc…. The cycle is broken by opening the sinus outflow tract and thinning the mucous so the infected material can drain (decongestants, steroids, mucolytics, nasal saline rinses) and by eliminating the infection (antibiotics). Attention must also be paid to the underlying condition that made the patient predisposed to acute sinusitis.
Why Do I Have Chronic Sinusitis?
This is the “million dollar question” that rhinologists, allergists, immunologists and ear, nose and throat doctors all over the world are trying to answer. Remember, sinusitis means inflammation of the sinus mucous membrane. The cause for chronic sinusitis is probably multifactorial. It seems that many patients with chronic sinusitis actually have an overactive immune response to inhaled foreign particles. This can be in the form of a “true allergy” confirmed by blood or skin allergy testing or an “allergic-like” response (when the problem clinically behaves like an allergy but the allergy tests are negative). Some researchers believe the chronic inflammation is due to certain bacteria residing in the nose and sinuses which cause a chronic infection that is resistant to standard treatments because they have formed a sticky protective blanket (biofilm) shielding the bacterial cells from antibiotics, nasal rinses and sprays. Others believe that bacteria in the nose and sinuses secrete a toxin ultimately leading to inflammation in the sinuses. Multiple reports also point to inhaled fungal spores, and the body’s reaction to them, as a cause for persistent inflammation. Some patients may have other medical conditions predisposing them to chronic sinus inflammation or infection (Cystic Fibrosis, Wegener’s Granulomatosis, Sarcoidosis, HIV/AIDS, Kartagener’s Syndrome, immunodeficiencies). A patient’s unique nasal and sinus anatomy (narrow drainage pathways, deviated septum, extra obstructing sinus cells) may also result in inefficient sinus mucous drainage and subsequent recurrent or persistent inflammation.
Every sinusitis patient is unique and therefore deserves a thorough evaluation by a physician experienced in the diagnosis and treatment of acute and chronic sinusitis. Because the etiology of sinusitis is often multi-factorial, several treatment modalities exist. Treatments are recommended and prescribed based on the patient’s specific contributing factors. Patients are best served by a dedicated, meticulous evaluation and treatment plan rather than a “cookie-cutter” or generic approach to therapy.
Thyroid Eye Disease and the Sinuses
More information coming soon ... check back.
Our Philosophy
Professionalism, Precision, Pride…
We believe in continued learning, unrelenting refinement of technical skills, patient education and the ultimate goal of making every patient that walks through our doors “feel better.” Our approach to certain conditions…
Chronic Sinusitis
This is first and foremost a medical disease. The inflammation in the mucous membrane ofmost forms of chronic sinusitis is similar in nature to the inflammation that occurs in the airways of asthmatics. These conditions are best managed with appropriate medical therapy aimed at blocking the inflammatory response to inhaled particles and eliminating secondary bacterial infections. Surgery does play a role in management of chronic sinusitis if medical therapy has failed to adequately improve the patients symptoms. Sinus surgery does not cure chronic sinusitis. It facilitates the medical treatment of the disorder by opening the sinuses, removing obstructing bony walls and polyps and washing out the sinuses. Medical therapy should be continued following sinus surgery to help prevent recurrence of severe inflammation and symptoms.
Nasal and Sinus Tumors
State of the art technology and instruments are utilized by the physicians at Arizona Sinus Center to decrease post-operative healing times, improve functional outcomes and decrease complications. Computerized surgical navigation, specialized endoscopes and a new generation of sinus instruments are utilized. For patients with nasal or sinus cancer, we often work closely with our colleagues in oncology, neurosurgery, head and neck cancer surgery and prosthodontics to provide outstanding multi-disciplinary care.
Nasal Obstruction
The key to effective treatment of nasal obstruction is making the correct diagnosis. A facial, nasal and upper respiratory exam is critical during the diagnostic evaluation. Nasal endoscopy or CT scanning may be required. Our physicians utilize both in-office treatments and operating room surgical procedures to improve nasal breathing.